Date Published: 8 Aug '23
Date Published: 8 Aug '23
Joints are where the ends of bones form a natural hinge or rub against each other, allowing the body to move. When we are young, the ends of our bones are covered in smooth articular cartilage that allows low-friction gliding. There are also ligaments, muscles and tendons surrounding the joint, holding the bones together and keeping the joint stable.
Joints also have a sack-like ‘synovial’ lining. This lining contains a thick ‘synovial fluid’ that fills the joint and helps keep it lubricated. The articular cartilage does not have access to the body’s blood supply but instead gets the nutrients it needs from the synovial fluid that surrounds it. Each time the joint moves, the cartilage compresses and expands, a bit like a stiff sponge. This compression and expansion ‘breathes’ the synovial fluid in and out, nourishing the cartilage.
.jpg)
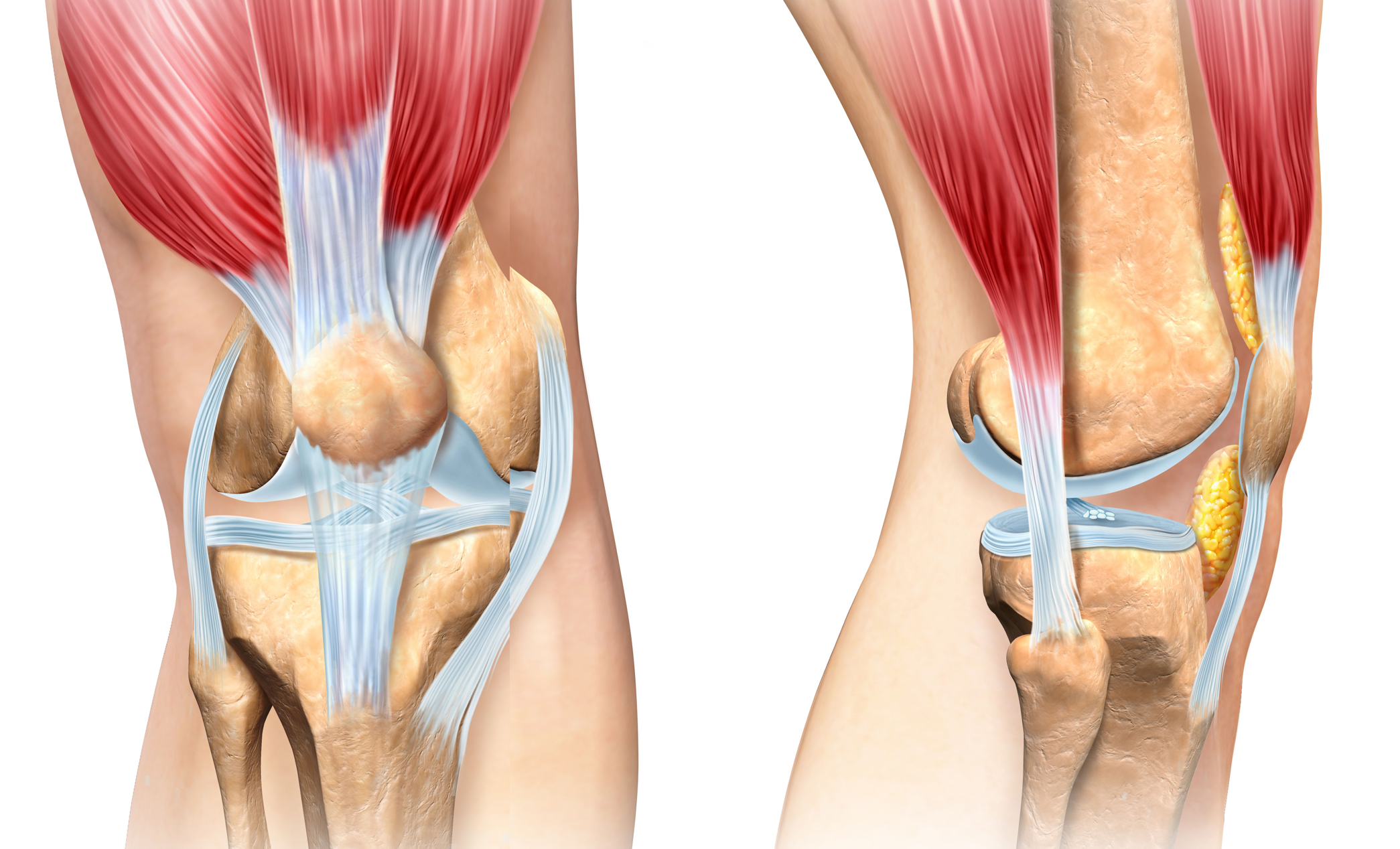
In describing the different areas of the knee joint, we divide it into three compartments that we assess individually:
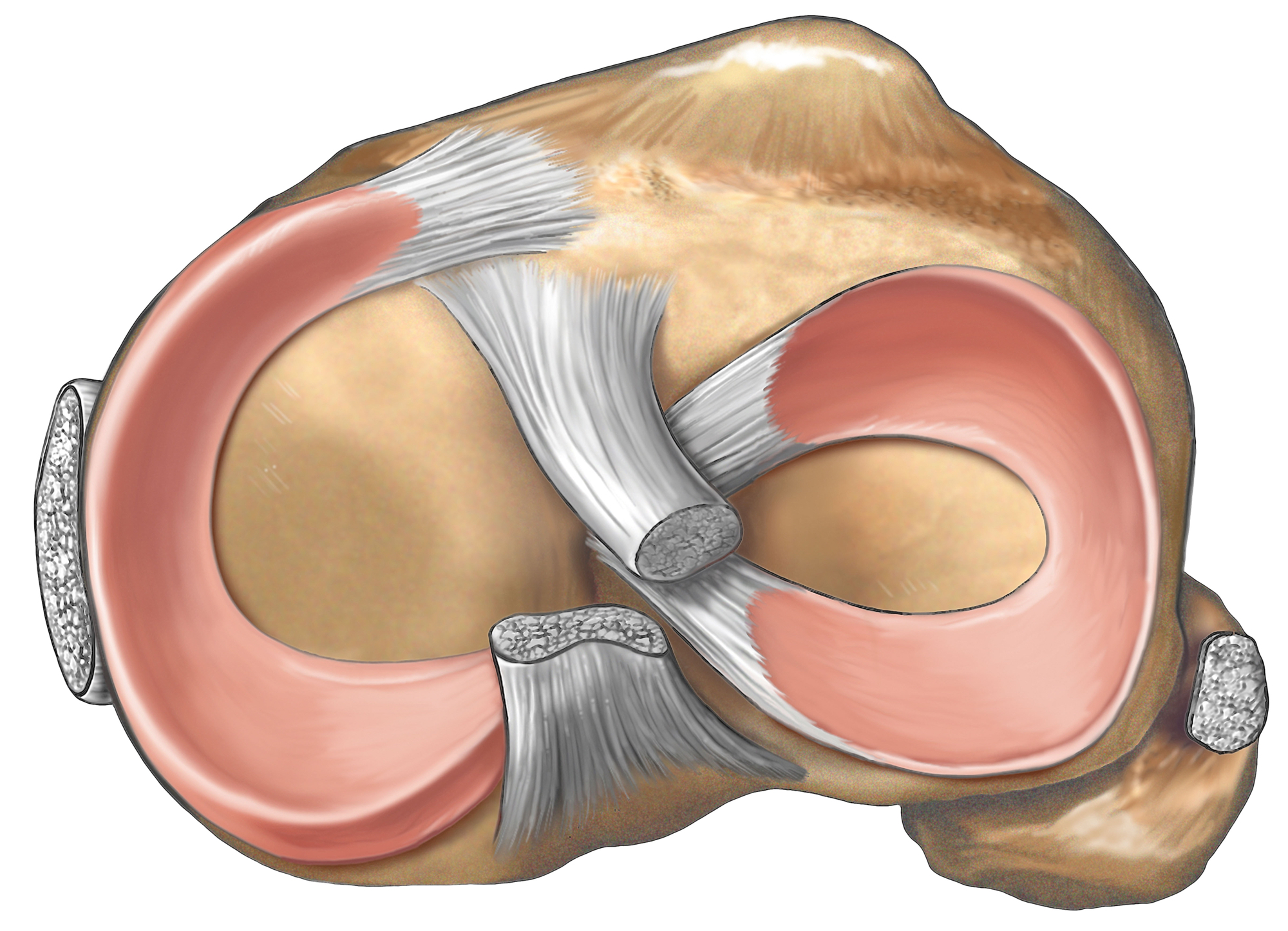
In this image, you can also see a side-on view of the ‘meniscii’. These are semicircular pieces of tissue attached to the tibia (shin bone) in both the medial and lateral compartments. The picture below shows these better, as the femur (or thigh bone) has been removed to look at the top of the tibia and the meniscii.
You may have heard the meniscii referred to as cartilage, but it is important that you know the difference between the meniscus cartilage and the articular cartilage which covers the end of the bones.
A meniscus is made of similar material as articular cartilage. Both are very tough tissue, but their purpose and the way they work is very different. Articular cartilage provides a gliding surface for the joint, whereas the menisci are there to share bodyweight through the knee joint rather than have it all focused on a small area of articular cartilage. In doing so, the meniscus helps protect and preserve the articular cartilage and cushion the load on the knee joint.
You will also see two ligaments in the middle of the knee called the cruciate ligaments, and a ligament on each side of the knee called the collateral ligaments. These ligaments all help stabilise the knee.
Surgical treatment of OA can be very successful but only for carefully selected patients.
Surgery performed on a patient for who it is inappropriate can be an inconvenient and expensive waste of time, or in some situations can actually make matters worse.
Arthroscopic surgery, or ‘cleaning out’ the knee joint, is an operation that has been commonly performed for OA for many years. However, in recent years, almost all evidence suggests it has no real benefit for knee OA.
Knee replacement surgery is a very successful operation but is only appropriate for people suffering from advanced OA who have already tried all the non-surgical options available. A small percentage of patients with very specific patterns of OA may be suitable for knee realignment or reconstruction surgery.
One of the keys to achieving success with surgical management is appropriate patient selection and timing of surgery. Our clinicians can
advise you on such matters and refer you to a knee surgeon when appropriate.
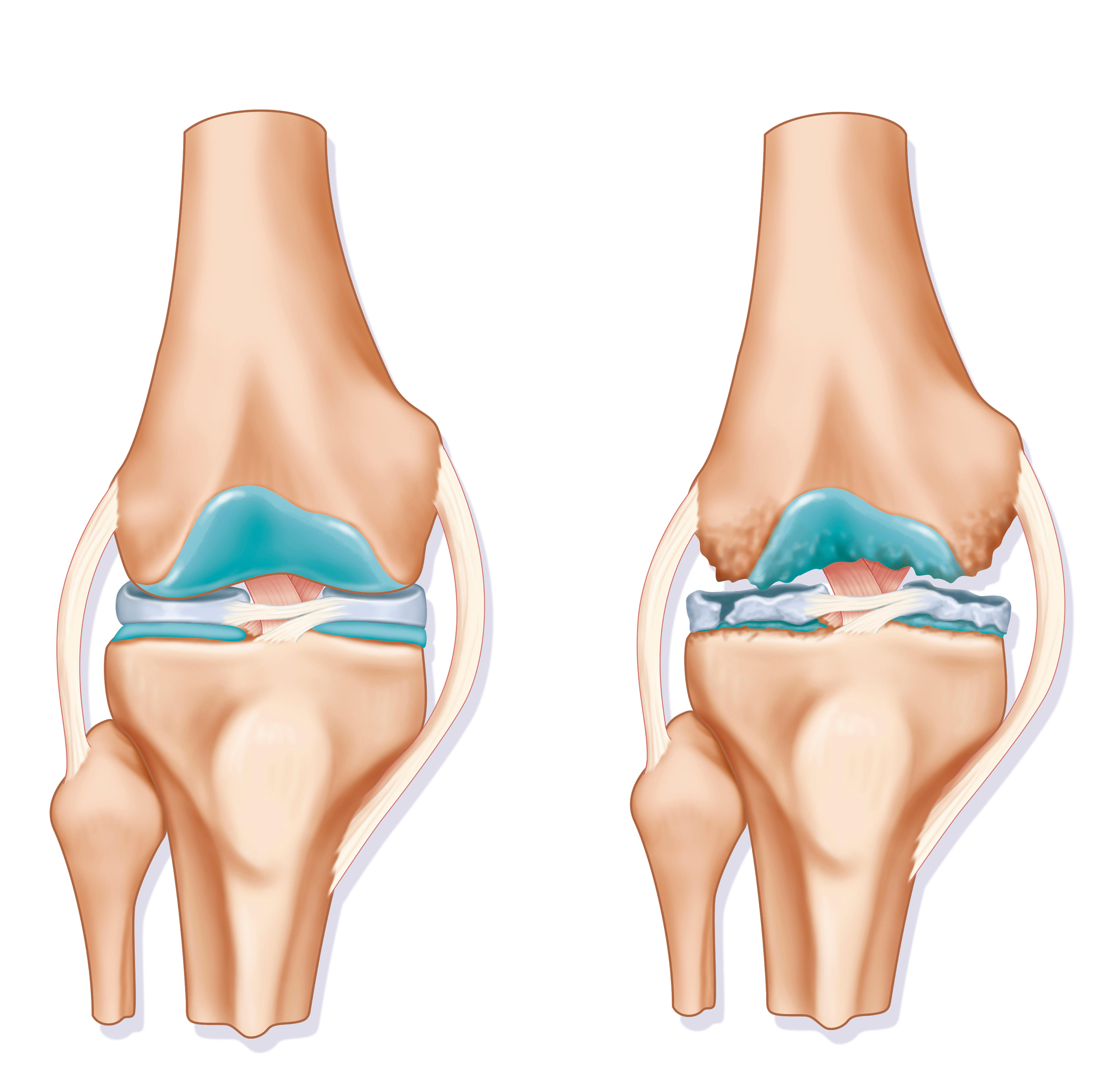
Osteoarthritis (OA) of the knee most commonly starts with damage to the articular cartilage, the meniscus, or both. This can occur through simple overloading of the joint by being overweight, from acute injuries to the knee, or from a combination of both. Having a family history of arthritis also increases the risk of developing OA. In the human knee joint, the medial compartment is the most likely to succumb to OA because it experiences the highest loads and, as a result, is also the most likely part of the knee to be injured.
Whereas other parts of our body heal back to their original state after an injury, articular cartilage and the meniscal cartilage do not. This means the damage to these structures can accumulate over time. The articular cartilage can become rougher and thinner, and the meniscus frayed and torn. This results in more friction and less cushioning between the ends of the bones and in the joint in general.
Complex biochemical and biological changes begin to occur in the joint in response to friction and damage, producing inflammation. If not well managed, the inflammation can gradually affect all the surrounding structures of the joint, causing pain and stiffness.
Pain and other symptoms from knee OA can come and go over time. Certain conditions may trigger painful ‘flare-ups’, such as cold weather,
small traumas to the joint, being inactive for a prolonged period of time, or biochemical changes in the body or joint. Sometimes, the
sufferer may be tricked into thinking that they have ‘cured’ their OA when it is being well managed, only to be disappointed by a flare-up
that seems to occur for no obvious reason.
Of course, the exact nature of the OA, its causes and the way it impacts on each sufferer’s life differs. Similarly, the way a person addresses their OA changes the way the disease will progress and impact their future. Generally, the earlier OA is addressed, the better the long-term outcome will be for the patient.
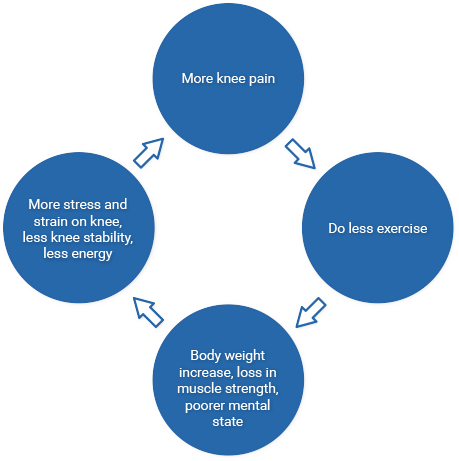
One of the most commonly reported responses early in the development of OA is that the patient reduces their physical activity due to the pain in their joint. This seems rational to most people, but it is actually the beginning of a vicious cycle of joint degradation and decreasing quality of life.
Let us explain.

Remember that OA is caused by cumulative injury and excess stress on the joint. Injuries can be small and go largely unnoticed, or be large and have a significant impact on your life.
Most people recall that when they were younger, fitter and active they injured themselves less and recovered faster. This is a normal
response and being young is certainly a major factor. However, it is also important to note that the more exercised our muscles, tendons,
ligaments and bones are, the stronger and more injury-resistant they are – regardless of our age.

A decision to decrease exercise will mean a loss of muscle strength and tone around a person’s joints and an increased risk of injury. A person can end up feeling they have insufficient strength in their knee and that it is increasingly becoming unstable or might ‘give way’.
Excess stress on the knee joint is most commonly caused by being overweight. Of course, a person’s decision to do less exercise because of their knee pain can often in turn lead to weight gain. It is tempting to think an extra kilogram here or there doesn’t make much difference, but that could not be further from the truth.
Due to the way our body mechanics work, an extra five kilograms of body weight will mean an extra twenty kilograms going through a painful knee during certain activities. Hip joints experience even more impact.
Less exercise also means your articular cartilage has less synovial fluid and nutrient moving through it. This will further reduce the
health of the damaged tissue, perhaps causing it to deteriorate faster.
Finally, a reduction in exercise has a significant impact on a person’s wellbeing. Regular exercise has been shown to have a positive impact on a person’s mental state. Not being able to exercise has the opposite effect. An inability to participate with friends and family in physical pursuits has a particularly negative impact on a person’s self-image and confidence.
Excess body weight, reduced muscle strength, less joint stability, deteriorating articular cartilage and a decline in mental health all contribute to an increase in pain for the OA sufferer and an increase in the rate of deterioration of the knee. The sufferer, in turn, does less exercise as a result of these factors and enters a destructive ‘vicious cycle’.
OA is not a complex disease to manage in its early years, but if these vicious cycles take hold and a patient’s overall health continues to decline, it can rapidly become part of a more complex condition. Eventually, all of the articular cartilage can be eroded from the ends of the bones. Some joint deformity, often with associated knee instability, can start to set in.
At this late stage, life will be very difficult for the sufferer. Simple tasks such as getting out of a low chair or driving a car can become close to impossible. The heavy emotional and mental impacts of this poor phyiscal health can also make the sufferer feel isolated and low.

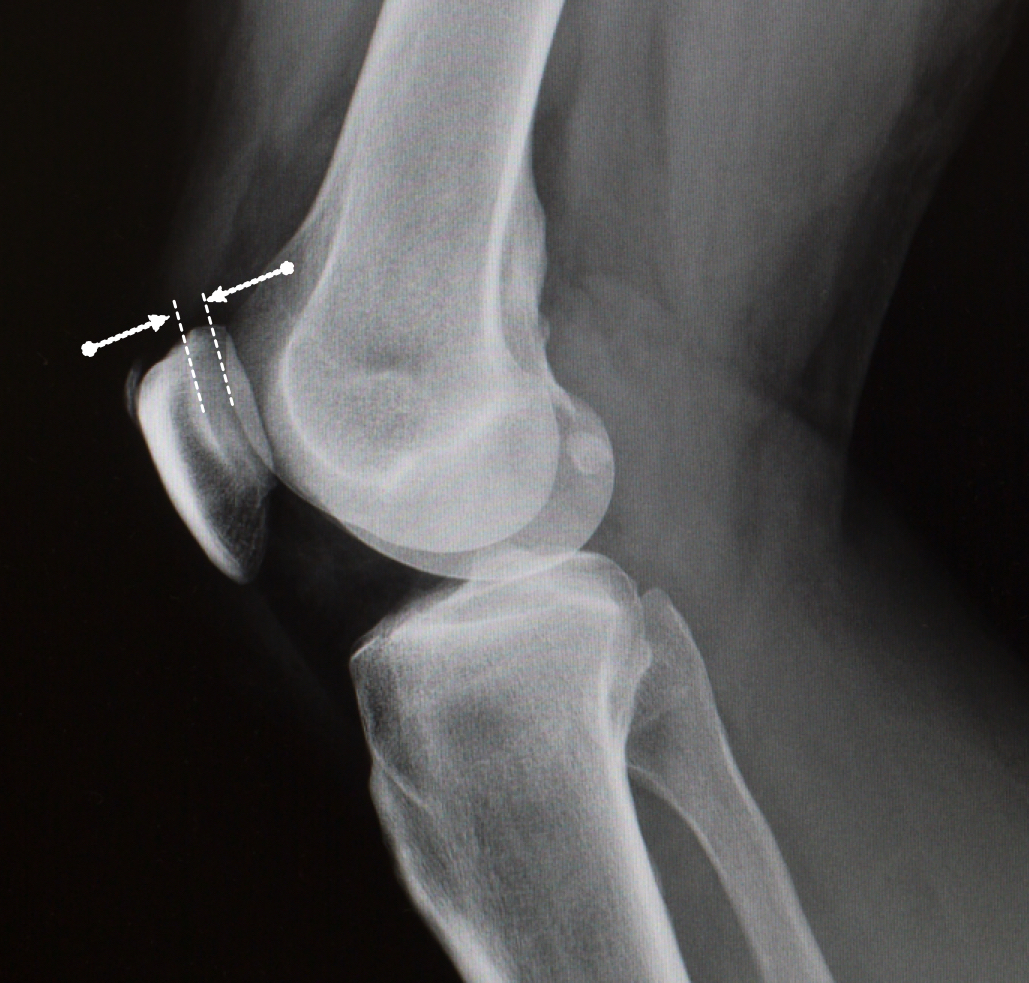
The articular cartilage and meniscus cannot be seen on an X-ray image. An X-ray of a healthy knee with good cartilage should show a gap between the bones, such as the knee on the right of this image.
You can see that there is no gap between the bones of the knee on the left of the image. This indicates the articular cartilage and meniscus have completely worn away causing arthritis and the ends of the bones to rub. This is a painful condition.
Osteoarthritis between the patella (knee cap) and femur (thigh bone) is also common. This lateral (side-on) X-ray shows a healthy gap
between the patella and femur, meaning the articular cartilage still has a healthy thickness. A narrowing of this gap would indicate
cartilage wear and osteoarthritis of the patella-femoral joint.

This X-ray shows cartilage wear in the medial compartment, or inside-knee, only. This kind of uneven wear can give the patient the appearance of being ‘bowlegged’ over time as the medial joint space collapses.
Wear on the outside or lateral compartment only can bring about the reverse appearance of having ‘knock knees’.
Our friendly staff are always here to help. Contact us to begin your journey to a happier, healthier you.